After a long year of challenges, we are finally approaching a potential turning point in the COVID-19 pandemic with the arrival of the first wave of vaccines. This post will introduce the science behind these vaccines and discuss some of the common questions related to this topic.
How Do Vaccines Protect Against Viruses?
Vaccines work against viruses by prompting the immune system to generate antibodies to defend against them. Viruses, including COVID-19, are coated with specific proteins that allow them to attach to our cells. These proteins are known as antigens because antibodies get generated in response to them.
The antibodies circulate in the blood and bind the exposed proteins on the surface of the virus. This process neutralizes the virus by preventing it from attaching to our cells. A signal travels to nearby white blood cells, which engulf and destroy the captured virus.
Vaccines work by:
- Introducing only the specific coat proteins of a virus.
- Triggering the protective antibody response without resulting in an actual infection.
- Allowing exposure to the virus that no longer results in infection.
As a result, vaccinated people have immunity to a specific infection.
The First Two mRNA Vaccines to Receive Emergency Use Authorization
The first two COVID-19 vaccines to receive emergency use authorization from Western governments are the mRNA-based products from Pfizer and Moderna. Both of these vaccines require a two-shot sequence with the second vaccination scheduled after 21 days (Pfizer) or 28 days (Moderna).
Based on current data from clinical trials consisting of nearly 44,000 people (Pfizer) and 30,000 people (Moderna), both vaccines’ efficacy is greater than 94%. There were no serious adverse events reported during the trials, and public immunization with these products has been ongoing since early December 2020.
A Third Vaccine Approved in The UK Uses a Viral Vector
A third coronavirus vaccine made by AstraZeneca was approved by UK regulators on December 30th. AstraZeneca’s product uses a viral vector rather than the mRNA-based technology. This is simply a different way to manufacture vaccines using a different host virus to introduce the immunity.
Initial data suggests that it has an efficacy of approximately 70%, but it also has a lower cost per dose and can be stored under typical refrigeration instead of the sub-zero temperatures needed for the mRNA products.
What Types of Side-Effects Could I Experience After a COVID-19 Vaccine?
A significant portion of the recipients reported mild flu-like symptoms such as fatigue and headache the day after receiving their second shots; however, this is a sign of the vaccine generating an appropriate immune response rather than an adverse reaction.
Like any other vaccine or medication, some patients may experience symptoms of an allergic reaction after receiving a COVID-19 vaccine. Newly released data confirms that serious reactions such as anaphylaxis are very rare, and there have only been 21 cases reported out of the nearly 2 million vaccinations administered thus far.
Allergic reactions can be managed effectively with medications, and all patients recovered without incident after receiving treatment. The CDC has reiterated that the benefits of immunization outweigh any potential risk of a treatable allergic reaction.
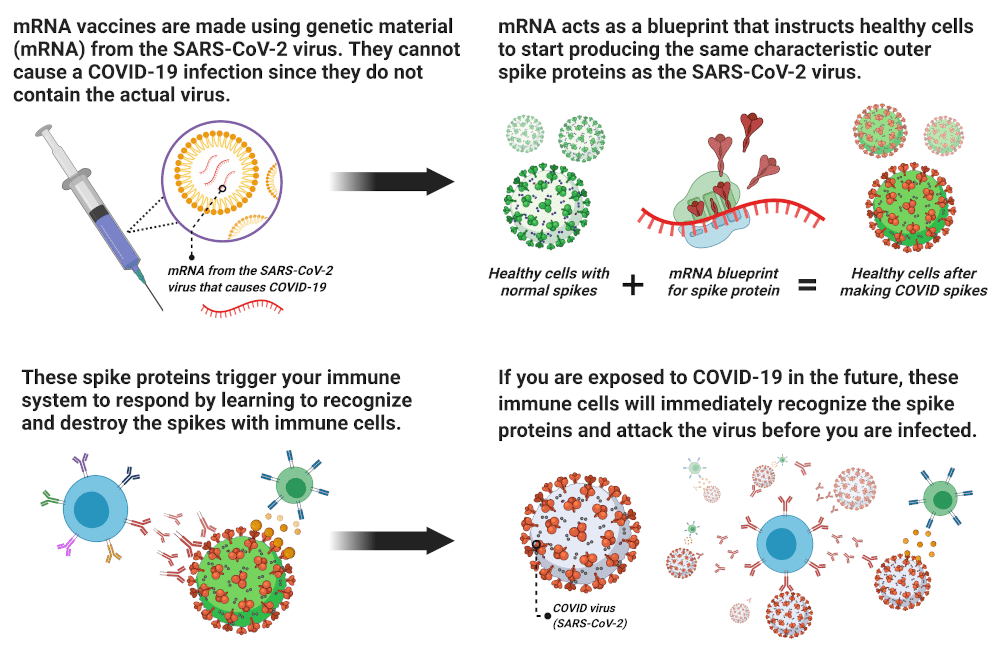
How Do mRNA Vaccines Create Immunity Against COVID-19?
Is It Possible to Get COVID-19 From the Vaccine?Â
No. It is not possible to become infected with COVID-19 from any of the vaccines.
Is It Possible for the mRNA Vaccine to Interfere With My DNA?
No. The mRNA in the vaccine breaks down and disappears from your body within a few days of receiving the vaccine. Your genetic material (DNA) is stored in a different part of the cell, and the mRNA cannot come into contact with your genes or alter them in any way.
The sole purpose of the mRNA is to provide a blueprint for the antigen protein to trigger your immune system and initiate the process of developing immunity to the virus.
How Long After the Vaccine Will I Develop Immunity, and How Long Will It last?
Based on preliminary analysis, the belief is that the vaccine will initially confer immunity approximately ten days after the first dose.
We do not know precisely how long immunity will last at this time because there is no data beyond the present to make an assessment. However, several promising studies have come out in recent months that indicate that immunity to severe COVID-19 infection may last many months or even years after immunity develops.
Expect significant research into this question in the months and years to come.
How Many People Will Need to be Vaccinated Before We Can Return to Normal Activities Again?
At this time, scientists estimate that approximately 75% of the population will need to receive the vaccination before normal activities such as going to the movies or holding a large gathering can safely resume.
Will I Still Need to Wear a Mask After I Am Vaccinated?Â
Yes, for the time being. It may take approximately one year to vaccinate the majority of the country. Masking and distancing should be maintained until federal and state health authorities have issued other recommendations.
Is It Safe to Get Both a Flu Vaccine and COVID Vaccine?Â
Yes. There is no known elevated risk from receiving both vaccines, and experts strongly recommend them to reduce the risk of severe illness and prevent overburdening of the healthcare system.
I Am Relatively Young and Healthy, Wouldn’t It Be Better to Just Get COVID-19 and Recover?
No. COVID-19 has been associated with many life-altering complications in all age groups including:
- Heart failure.
- Kidney failure.
- Strokes
- Irreparable lung damage.
- Severe neurological or cognitive disorders resulting in memory loss, chronic fatigue, and other debilitating symptoms.
In one study of 3,222 young adults between the ages of 18 – 34 who were hospitalized for COVID-19 in the US, 20% required ICU care and 3% died. Additionally, many of the chronic manifestations of COVID-19 are only beginning to be identified.
The vaccine is safe and effective, and it is a much better alternative to seeking immunity through infection given the high risk of complications from the disease. Also, the vaccine is known to provide immunity for much longer than infection and recovery, which may only provide protection for 1-3 months.
I Have Already Had COVID-19, Do I Need to Get the Vaccine? Â
Yes. While previous infection with COVID-19 does confer some natural immunity, that immunity is thought to last only a short time. The two-shot series of vaccines produce a much higher immune response that is longer lasting than the immunity conferred by a previous infection.
Are You Ready to Develop A Plan To Protect Your Employees From COVID-19?
Although the COVID-19 vaccine is approved, no one knows how long it will take for pharmaceutical companies to produce enough doses to vaccinate most of the global population.
In the meantime, your company should take precautions. Consider working with a COVID-19 Services partner experienced in keeping employees and communities safe through screening, testing, and consulting services that can soften the pandemic’s effect on your company.
Keep Employees Safe
References:
Cunningham JW, Vaduganathan M, Claggett BL, et al. Clinical Outcomes in Young US Adults Hospitalized With COVID-19. JAMA Intern Med. Published online September 9, 2020. doi:10.1001/jamainternmed.2020.5313
Jeyanathan M, Afkhami S, Smaill F, Miller MS, Lichty BD, Xing Z. Immunological considerations for COVID-19 vaccine strategies. Nat Rev Immunol. 2020;20(10):615-632.
Le TT, Andreadakis Z, Kumar A, et al. The COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19(5):305-306.
“Types of Vaccines†Infographic. BU Epidemiology COVID-19 Response Corps. Accessed December 10, 2020. https://sites.bu.edu/covid-corps/projects/science-communication/types-of-vaccines infographics/
Coronavirus disease (COVID-19): Vaccines. Accessed December 10, 2020. https://www.who.int/news room/q-a-detail/coronavirus-disease-(covid-19)-vaccines
CDC. Understanding mRNA COVID-19 Vaccines. Published December 3, 2020. Accessed December 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/mrna.html
Poland GA, Ovsyannikova IG, Kennedy RB. SARS-CoV-2 immunity: review and applications to phase 3 vaccine candidates. Lancet. 2020;396(10262):1595-1606.
CDC. Understanding How COVID-19 Vaccines Work. Published December 10, 2020. Accessed December 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/how they-work.html
CDC. Different COVID-19 Vaccines. Published December 3, 2020. Accessed December 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines.html