The COVID-19 pandemic has impacted nearly every aspect of our lives in and out of the workplace. As we approach the flu season’s start, it is crucial to consider the potential impacts of a widespread flu outbreak alongside the COVID-19 epidemic in the United States and globally.Â
This blog post will:
- Provide an overview of the similarities and differences between the two viruses
- Discuss the burden of influenza in the context of occupational and industrial health settings
- Highlight some of the evidence-based strategies for mitigating these impactsÂ
Our medical experts know how important it is for your organization to ensure the lowest possible risk and maintain operational continuity in this unprecedented time.Â
The Similarities and Differences
The diagram below illustrates some of the most significant similarities and differences between COVID-19 and seasonal flu.
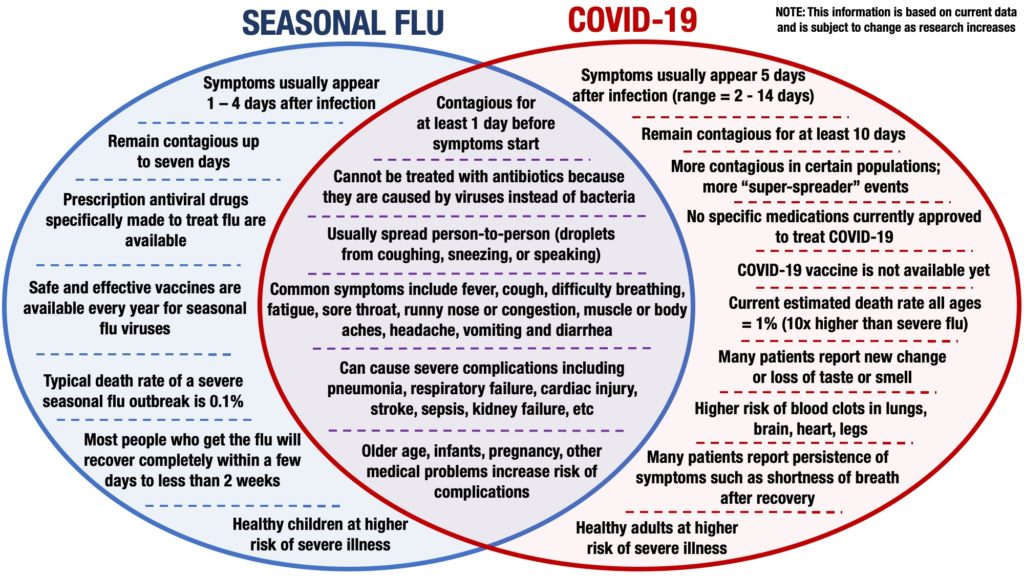
The overlap in clinical appearance between the two illnesses is likely to pose significant challenges from a clinical and occupational health and safety standpoint. Patients who have flu-like symptoms may be infected with influenza, COVID-19, or both viruses simultaneously in co-infection cases.Â
Symptomatic individuals or close contacts will need to be managed as presumptive COVID-19 cases unless proven otherwise. This situation may require extended isolation periods and additional testing beyond what doctors require for influenza alone.
Seasonal Influenza Outbreaks Already Cause Significant Impacts in the United StatesÂ
The annual impact of seasonal flu outbreaks in the United States is sizable from social, economic, and public health perspectives.
According to the Centers for Disease Control (CDC), as many as 56 million flu cases resulted in 26 million medical visits, 740,000 hospitalizations, and 62,000 deaths between October 2019 – March 2020 in the United States alone.
It is believed that the flu accounts for at least 10% of all employee absences due to illness in the US. The total economic burden of seasonal influenza in the United States is difficult to calculate, but recent studies have estimated an annual cost of $16 billion USD and over 20 million days of lost worker productivity.
The Costs of Widespread Illness
Most of these costs are attributed to the financial impact of worker absence due to illness rather than the direct costs of medical care.Â
Aside from the direct effects, there is significant concern about the second-order effects that would result from a substantial flu outbreak this year. It is not uncommon for hospitals to approach the maximum capacity of ICU beds and ventilators during the annual surge of influenza patients.Â
In many US areas, the current strain on the healthcare system caused by COVID-19 has exhausted those resources. A severe season this year could result in a “twindemic†of COVID-19 and influenza that could overwhelm the capacity of the US healthcare system to provide the necessary level of care to patients with significant respiratory illnesses.
Risk-reduction Strategies for the Coming Flu Season in 2020Â
The risks posed by a severe flu season in the context of the current COVID-19 pandemic are significant, and the most effective means of reducing these risks is prevention. The first line of defense against seasonal flu is vaccination, and the effectiveness of immunization increases with the number of individuals who receive the vaccine.Â
The flu vaccine formulation is adjusted each year to target the 3 – 4 strains believed to pose the highest risk of a widespread outbreak. Recent studies indicate that the flu vaccine reduces the risk of illness by 40% – 60% when it is well-matched against the circulating strains of flu.Â
In an Occupational Setting
In the occupational setting, one study from the UK reported that flu immunization halved the number of illnesses in vaccinated versus unvaccinated workers. Increasing the employee vaccination rate is a simple way to make a significant positive impact, as studies have reported that only 28% of workers in the United States receive annual flu vaccines.Â
Vaccination is an important first line of defense, but non-pharmaceutical interventions are equally important in preventing serious flu outbreaks. Researchers have identified five non-pharmaceutical interventions of particular importance for reducing the risk of virus transmission during a pandemic:Â
- Basic hygiene and respiratory etiquette
- Disease surveillance
- Capabilities for rapidly diagnosing viral infections
- Widespread use of masks and other personal protective equipment (PPE)
- Isolating sick individuals as well as close contacts
The importance of even basic interventions cannot be overstated. Occupational health studies on the implementation of hand-hygiene programs combining education and alcohol-based hand sanitizer use in the workplace have reported decreases in absenteeism by 20% and self-reported symptoms of respiratory or gastrointestinal illness by 30%.Â
Similar Studies in a Different Setting
A similar study conducted in an educational setting reported that the use of alcohol-based hand sanitizers in university dormitories resulted in a 40% reduction in respiratory illnesses and a 43% decrease in missed school days. Â
The basic steps required to reduce the risk of a serious flu season are the same as those recommended for reducing the spread of COVID-19. The precautions taken to protect against COVID-19 may have a secondary benefit of reducing the impact of the coming flu season, but widespread adoption will be needed to achieve the maximum benefit.Â
Employers should implement proven strategies including:
- Screening
- Testing
- Encouraging employees to obtain seasonal flu vaccinations every year
- Targeted hygiene interventions – hand sanitizer stations
Individuals who have been vaccinated or tested negative should be reminded to continue practicing the fundamental components of infection control including:Â
- Handwashing
- Masking
- Social distancing